Though lifesaving, liver tumor surgeries are complex. In addition the risks associated with surgeries in general—such as pain and reactions to anesthesia—liver surgeries can cause drops in blood count due to the liver’s key role in regulating blood clotting. Although these complications may be fewer in laparoscopic liver surgeries than in open surgeries, laparoscopic solutions remain uncommon.
Virtual reality (VR) training systems can help surgeons train and plan for laparoscopic procedures by placing them in a similar headspace, enabling them to practice the types of decisions they will make during the operation, providing planning space ahead of a procedure, and allowing trainees to improve their psychomotor and communication skills. Lawrence Livermore postdoctoral researcher Vuthea Chheang led an effort to develop a virtual training hospital for laparoscopic liver surgery, which the team published in the journal Computers & Graphics.
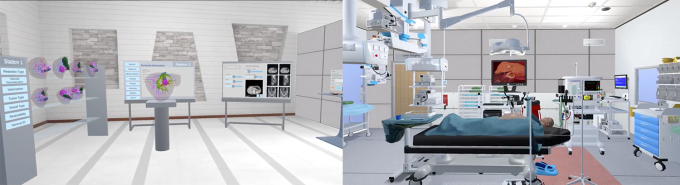
Chheang’s virtual hospital is extensive, requiring multiple participants to go through every step of the surgical process together—from meeting one another in the lobby, to preoperative planning in the virtual surgical planning room, to completing a laparoscopic surgery simulation in the virtual operating room. In the planning room, the surgeons have access to a virtual organ library, an imaging simulator, and more, allowing them to determine the proper surgical resection and its impacts on the organ for each specific case study. When they move into the operating room, they have access to two sets of physical training aids—one for the lead surgeon to use for cutting and grabbing liver tissue, and the other for the assistant surgeon in charge of the laparoscopic camera—to ensure the platform allows surgeons to practice their psychomotor skills.
Though desktop applications are common tools for liver surgery training, previous approaches are less realistic than Chheang’s prototype. Most are two-dimensional rather than VR-based and, critically, they do not enable collaboration between surgeons. In contrast, the virtual surgical training platform developed by Chheang and his team presents trainees with realistic scenarios that require collaboration among the surgeons for a successful outcome. “In a real setting, the surgeons need to communicate with the anesthesiologist,” Chheang says.
For example, in some scenarios, it is the anesthesiologist’s responsibility to identify excessive bleeding and inform the surgeons. The bleeding may also block the laparoscopic camera, and the VR platform prepares the participants to work through such an issue. In another training scenario included in the platform, the patient’s muscles begin to tense and move, and the surgeons must work closely with the anesthesiologist to administer additional muscle relaxants and return the patient to an operable state.
The virtual training environment is ideally run with a senior surgeon leading the surgery, and two to three junior surgeons or medical students assisting or observing. Because they communicate via headsets, customized avatars, and real-time game synchronization, the participants can collaborate from different locations.
Virtual Solutions for Real Scenarios
Beyond the obvious training application, the platform can also be used for preoperative planning. While the game includes teaching data and organ models for trainees to use, “the liver is different from patient to patient, and the type of tumor is different. Some are more complicated than others,” Chheang says. To account for unique variations, surgeons can upload a specific patient’s real information and conduct a mock procedure with VR laparoscopic simulations to prepare for entering the real operation room.
The prototype is currently being used at a university hospital in Mainz, Germany. A pilot study with surgical residents and experienced liver surgeons has had generally positive results and indicated that the platform provides a reasonable foundation with significant advantages over other simulators. However, additional clinical evaluation is needed before the simulator can realize its full applications. “We’ve confirmed the technical feasibility, but the clinical feasibility also needs to be confirmed for training in the hospital,” says Chheang.
Based on constructive feedback from the pilot studies, the researchers are working to address remaining technical limitations of the VR platform, including making the deformation of the liver during simulations feel more realistic. Chheang emphasizes that regardless of the amount and quality of training, surgeons always need to be more cognizant of safety in the real world than in a simulation environment.
Beyond Surgery
At the Lab, Chheang is now working on applying similar VR technologies to mission area applications. In particular, Chheang is focused on VR for collaborative, virtual inspections in additive manufacturing, wherein scientists scan and upload a 3D printed part.
“The technology and the skillset are the same, but the topic can change,” he says. Previously, Chheang was also involved in a VR therapy project, noting, “I still apply that kind of technology at the Lab to see how it can help improve our workflows.”
He adds, “Augmented reality and VR technologies are really advanced now, and if we can apply them at the Lab, it will be a game changer—not only for manufacturing and printing but in many other work areas as well.”
Chheang collaborated with researchers from the University of Magdeburg in Magdeburg, Germany, and the University Medical Center of the Johannes Gutenberg-University Mainz in Mainz, Germany, on this project.
—Anashe Bandari